Breaking through the limit of light penetration depth, fiber optic therapy brings a revolution in cancer treatment
The International Agency for Research on Cancer estimates that 20% of people worldwide will develop cancer during their lifetime. Traditional surgery, chemotherapy, and radiotherapy are currently used as available clinical approaches for most cancer patients. Due to unavoidable resistance to drugs and radiation, traditional chemotherapy and radiotherapy have poor efficacy. As one of the emerging cancer treatment methods using light as the medium, photothermal therapy (PTT), in which nanomaterials absorb energy from photons and dissipate it partially in the form of heat to trigger the death of cancer cells, has attracted significant attention due to its noninvasive nature, high specificity and efficiency, and insignificant side effects. However, PTT still faces a major challenge, that is, the limited light penetration depth in the body. Considering the above problems, optical fibers provide the possibility of solving them. In the field of PTT, optical fibers can be used as a light guiding medium in vivo, thus greatly reducing light scattering and absorption in tissues and overcoming the obstacle of limited light penetration depth.
On November 29, 2023, Yunyun Huang, Bai-Ou Guan, Institute of Photonics Technology, Jinan University, China, and their team published a paper titled “Marriage of a Dual-Plasmonic Interface and Optical Microfiber for NIR-II Cancer Theranostics” in Advanced Materials. In this work, they reported a photothermal theranostic fiber integrating cancer detection and therapeutic functions.
The protein [Recombinant Alpha-Fetoprotein (AFP), RPA153Ra01] of Cloud-Clone brand was chosed in this article, we are so proud for supporting the reaserchers.
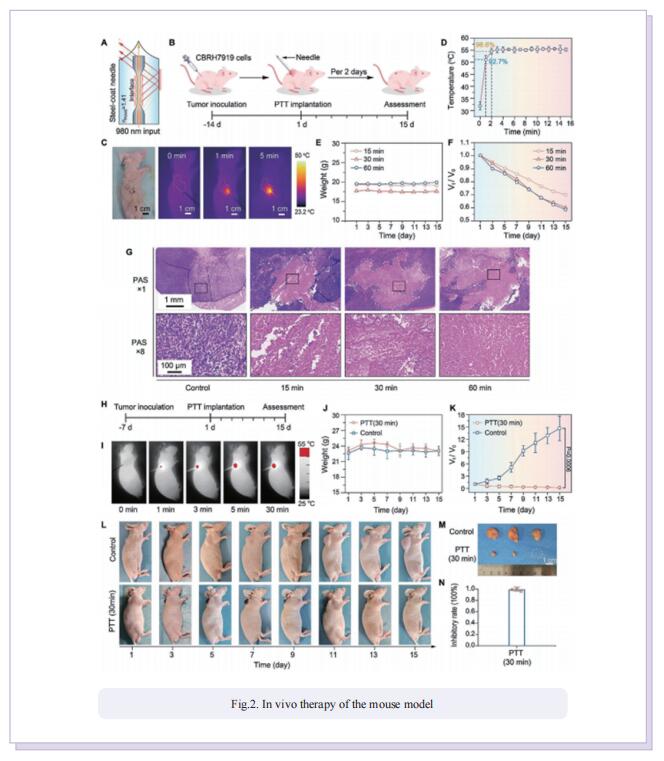
In this study, the authors propose a technique that combines the design concepts of optical fibers and photothermal agents via interface design. Using an optical microfiber as the PTT platform, photothermal agents were assembled on the microfiber interface to develop a PTT fiber. The photothermal effect of the interface materials enabled flexible temperature tuning of the fiber. Moreover, the real-time temperature of the fiber could be recorded by a fiber Bragg grating (FBG) at the side. The flexibility of the interface facilitated tuning of the temperature rise of the prepared fiber by between 0 °C and 90 °C. The heating effect can be detected and compensated by employing microfiber and FBG. Additionally, with the sensor nature of the optical microfiber, the prepared fiber could quantify cancer cells. Thus, the fiber could perform PTT on cancer cells and tumor tissues at the site where cancer cells were detected. In turn, it was capable of evaluating the PTT effect through quantification of the cancer cells by the optical microfiber sensor. The fiber, consisting of a dual-plasmonic nanointerface and an optical microfiber, can be used to distinguish cancer cells from normal cells, quantify cancer cells, perform hyperthermal ablation of cancer cells, and evaluate the ablation efficacy. Its cancer cell ablation rate reaches 89% in a single treatment. In vitro and in vivo studies reveal quick, deep-tissue photonic hyperthermia in the NIR-II window, which can markedly ablate tumors.
Taken together, a fiber with cancer cell detection and NIR-II PTT functions was developed. The marriage of a dualplasmonic nanointerface and an optical microfiber represents a different PTT concept with the potential to overcome the obstacles of limited light penetration depth and nonspecific accumulation in and accidental injury to normal tissues. It is hoped that this integrated theranostic platform may become a practicable strategy for simultaneous cancer diagnostics, therapeutics, and postoperative monitoring to accelerate the exploitation and clinical translation of intelligent theranostics.