New progress in the treatment of acute kidney injury
Acute kidney injury (AKI) is a global health problem, which affects about 20% of hospital inpatients. The primary clinical causes of AKI consist of sepsis, and nephrotoxic medications, ischemia-reperfusion injury. Current therapies for AKI are supportive, and short-term mortality remains high. In those who survive an episode of AKI, 30% are left with chronic kidney disease (CKD). The remaining 70% that recover full kidney function are at about 28-fold increased risk of ultimately developing CKD. Both AKI and CKD are strongly and independently associated with incident cardiovascular disease, and together, these exert a substantial global socioeconomic burden. Recently, a number of literatures have reported studies related to AKI, which may provide help for the treatment and prevention of related diseases.
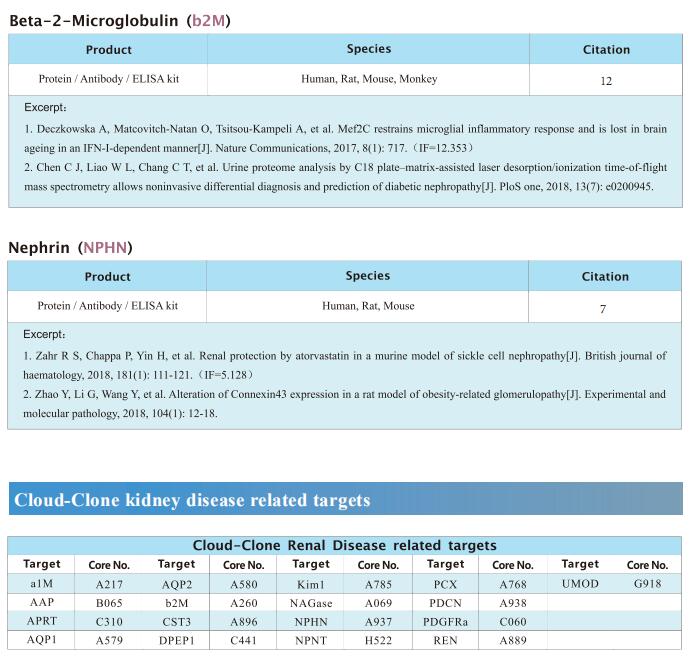
1. Endothelin blockade prevents the long-term cardiovascular and renal sequelae of AKI in mice
AKI is common and associated with increased risks of cardiovascular and chronic kidney disease. Causative molecular/physiological pathways are poorly defined. There are no therapies to improve long-term outcomes. Neeraj Dhaun, Department of Renal Medicine, Royal Infirmary of Edinburgh, UK, and his team found a causal role for activated endothelin system in the transition of AKI to chronic disease[1]. To show causality, AKI was induced in mice by prolonged ischemia. Ischemic injury resulted in hypertension, endothelium-dependent and endothelium-independent macrovascular and microvascular dysfunction, and an increase in circulating inflammatory Ly6Chigh monocytes. In the kidney, they observed fibrosis, microvascular rarefaction, and inflammation. Administration of endothelin-A antagonist, normalized blood pressure, improved macrovascular and microvascular function, and prevented the transition of AKI to CKD (Fig.1). Endothelin-A blockade reduced circulating and renal proinflammatory Ly6Chigh monocytes and B cells, and promoted recruitment of anti-inflammatory Ly6Clow monocytes to the kidney. Their studies suggest that existing drugs that block the endothelin system, particularly those coupling vascular support and anti-inflammatory action, can prevent the transition of AKI to chronic kidney and cardiovascular disease.
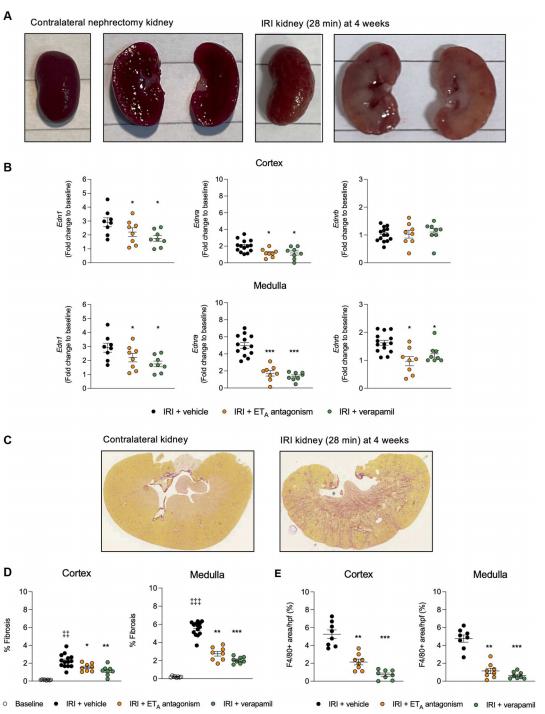
Fig.1 Endothelin-A receptor antagonism and verapamil protect AKI transitioning to CKD in mice
2. FFAR4 improves the senescence of tubular epithelial cells by AMPK/SirT3 signaling in acute kidney injury
Despite substantial progress in understanding the mechanism of AKI, no effective therapy is available for treatment or prevention. Liang Ma, Kidney Research Institute, National Clinical Research Center for Geriatrics and Division of Nephrology, West China Hospital of Sichuan University, China, and his team found that the expression of FFAR4 was abnormally decreased in tubular epithelial cells (TECs) of cisplatin, cecal ligation/perforation and ischemia/ reperfusion injury-induced AKI mice[2]. Systemic and conditional TEC-specific knockout of FFAR4 aggravated renal function and pathological damage, whereas FFAR4 activation by TUG-891 alleviated the severity of disease in cisplatin-induced AKI mice. Moreover, they found that FFAR4 regulated cellular senescence both in injured kidneys of AKI mice and TECs. Mechanistically, pharmacological activation and overexpression of FFAR4 reversed the decrease of aging-related SirT3 protein, where FFAR4 regulated SirT3 expression to exhibit anti-senescent effect via Gq subunit-mediated CaMKKβ/AMPK signaling in cisplatin-induced mice and TECs (Fig.2). These findings highlight the original role of tubular FFAR4 in cellular senescence via AMPK/SirT3 signaling and identify FFAR4 as a potential drug target against AKI.
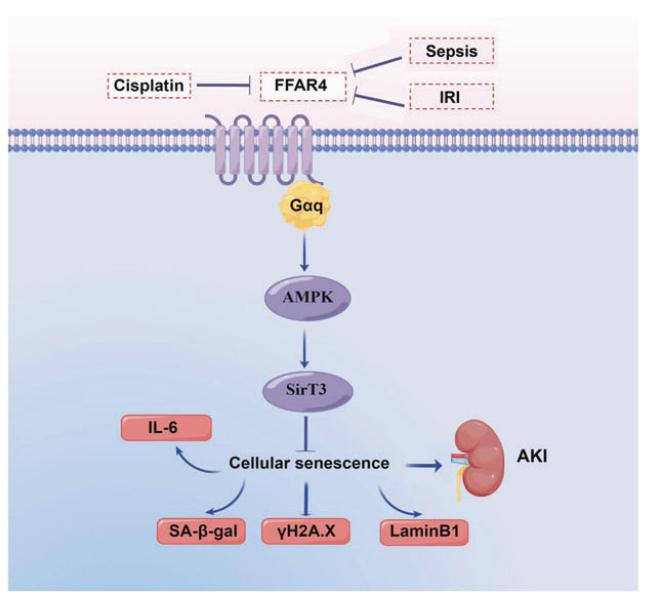
Fig.2 Schematic illustration of FFAR4 in cellular senescence of AKI
3. Unique Inflammatory Macrophage Subset as a Druggable Target for Alleviating AKI
Macrophages are the main effector cells of kidney inflammation. However, macrophage heterogeneity in ischemia reperfusion injury induced AKI (IRI-AKI) remains unclear. Ying Chen, Peking University Institute of Nephrology, China, and his team demonstrated the complementary roles of kidney resident macrophages (KRMs) and monocyte-derived infiltrated macrophages (IMs) in modulating tissue inflammation and promoting tissue repair by using single-cell RNA sequencing of the mononuclear phagocytic system in the murine IRI model[3]. A unique population of S100A9hiLy6Chi IMs is identified as an early responder to AKI, mediating the initiation and amplification of kidney inflammation (Fig.3). Kidney infiltration of S100A8/A9+ macrophages and the relevance of renal S100A8/A9 to tissue injury is confirmed in human AKI. Targeting the S100A8/A9 signaling with small-molecule inhibitors exhibits renal protective effects represented by improved renal function and reduced mortality in bilateral IRI model, and decreased inflammatory response, ameliorated kidney injury, and improved long-term outcome with decreased renal fibrosis in the unilateral IRI model. The findings support S100A8/A9 blockade as a feasible and clinically relevant therapy potentially waiting for translation in human AKI.
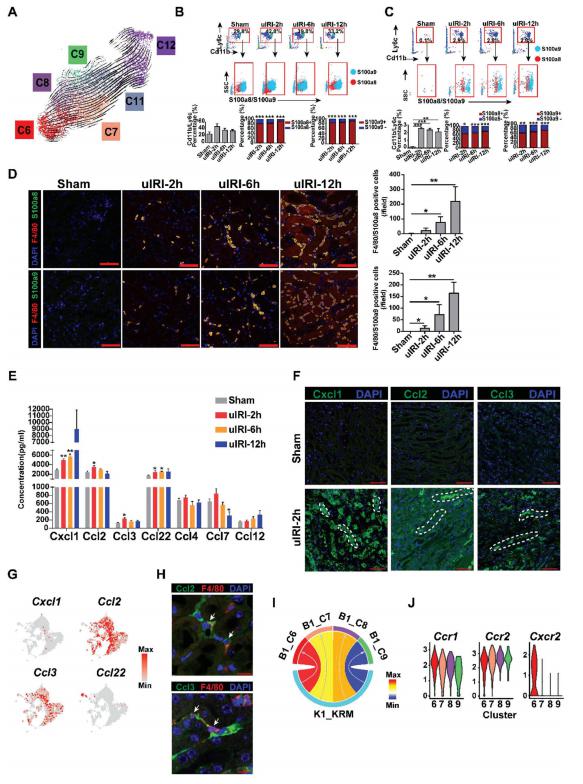
Fig.3 S100A9hiLy6Chi monocytes infiltration in response to kidney injury signal
References
[1]Czopek A, Moorhouse R, Gallacher PJ, et al. Endothelin blockade prevents the long-term cardiovascular and renal sequelae of acute kidney injury in mice [J]. Sci Transl Med. 2022;14(675):eabf5074. (IF=19.319)
[2]Yang L, Wang B, Guo F, et al. FFAR4 improves the senescence of tubular epithelial cells by AMPK/SirT3 signaling in acute kidney injury [J]. Signal Transduct Target Ther. 2022;7(1):384. (IF=38.104)
[3]Yao W, Chen Y, Li Z, et al. Single Cell RNA Sequencing Identifies a Unique Inflammatory Macrophage Subset as a Druggable Target for Alleviating Acute Kidney Injury [J]. Adv Sci (Weinh). 2022;9(12):e2103675. (IF=17.521)
Cloud-Clone can not only provide animal models of a variety of kidney diseases, including acute kidney injury, renal fibrosis, renal failure, glomerulonephritis, kidney stones, hydronephrosis and other common kidney diseases. We also have a variety of kidney disease related indicators detection products and the above endothelin A receptor, FFAR4, CaMKKβ, AMPK, SirT3, S100A8/A9 and other related products, which can help the vast number of researchers to carry out research on the treatment of kidney disease.